MBBS 8th semester
Name:Rithika.K
This is an online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
Case discussion
A 51 year old male patient came to the general medicine opd with a chief complaints of
Loss of taste and smell since 7 days
Cough since 6 days
Shortness of breath on exertion since 3 days
History of present illness:
Patient was apparently alright one week back then he developed loss of smell and taste later he developed cough which is of productive type and white in color initially later became green
He also developed shortness of breath on walking
Not associated with fever
No history of loose stools or vomitings
History of past illness:
K/C/O hypertension since 4 years
K/C/O type 2 diabetes
No other co-morbidities
Family history: non contributory
Personal history:
Appetite : normal
Diet : mixed
Bowel and bladder : regular
No known allergies
Addictions : regular intake of alcohol
Tobacco smoker
Treatment history:
Tab. Cinod t OD for hypertension
Tab. Glucoryl M1 for diabetes mellitus
Physical examination:
Patient was examined in a well lit room and the consent was taken
Patient was concious coherent and cooperative
Vitals: (02-05-2021)
Blood pressure: 140/90 mm Hg
Pulse rate: 110 per min
Temperature: 98.6 °F
SPO2: 98% at 6 liters of O2
Systemic examination:
Cardiovascular System:
S1 and S2 heart sounds heard, no murmurs.
Respiratory System:
Dyspnea is present
Centrally placed trachea
Normal Vesicular breath sounds heard
Per Abdomen:
Scaphoid shaped abdomen,no tenderness, no palpable mass, no organomegaly
Central Nervous System:Intact
On 03-05-2021(day 8 of symptoms)
Vitals:
Blood pressure:130/80 mmHg
Pulse rate: 84 bpm
Temperature: afebrile
SPO2: 94% on 2L of O2
GRBS: 268 mg/dl ( 8 units of HIA given)
Corad-5
CT severity-12/25
On 04-05-2021( day 9 of symptoms)
Vitals:
Blood pressure:140/70 mmHg
Pulse rate: 113bpm
Respiratory rate: 25 cpm
Temperature: 98.4°F
SPO2: 94% on 2L of O2
GRBS: 258 mg/dl ( 3 units of Inj.HIA given s/c)
Corad-5
CT severity-12/25
On 05-05-2021(day 10 of symptoms)
Vitals:
Blood pressure:130/80 mmHg
Pulse rate: 86bpm
Temperature: afebrile
SPO2: 97%
GRBS: 250 mg/dl
On 06-05-2021
Vitals:
Blood pressure:110/70 mmHg
Pulse rate: 86bpm
Temperature: 97.2°F
SPO2: 96%
GRBS: 247mg/dl
On 07-05-2021
Vitals:
Blood pressure:130/80 mmHg
Pulse rate: 105bpm
Temperature: 98.4°F
SPO2: 95% on room air
GRBS: 243 mg/dl
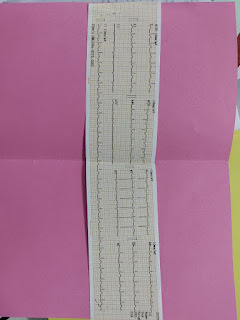
Investigations:
Provisional diagnosis: acute viral pneumonia secondary to covid 19 infection
Severity of covid- mild to moderate
Treatment:
Tab. AUGMENTIN 625mg
Inhalation to maintain SPO2 at >99%
Nebulization with BUDECORT 8th hourly and DUOLIN 8th hourly and MUCOMISE 12th hourly
Syrup.ASCORIL -10ml TID
Tab. PCM 650 mg
Inj.HAI Subcutaneously according to sliding scale at 8 am 1 pm and 8 pm
GRBS charting (6th hourly)
Tab.PANTOP 40 mg OD dose
Tab. CINOD-T OD dose
Monitor Temp/ BP/ PR /SPO2 2 hourly
Inj.CLEXANE 60mg subcutaneous OD dose
Tab.FLUVIR 75 mg BD
Patient was discharged on 07-05-2021 at 6:30 pm with rapid antigen test positive



Comments
Post a Comment