A 32 year old male with CKD on MHD
This is an online e log book to discuss our patient identified health data shared after taking his/her guardian signed informed consent. Here we discuss our individual patient problems through a series of inputs from available global online community of experts with a aim to solve those patients clinical problem with collective current best evidence based inputs.
This blog also reflects my patient centered online learning portfolio and valuable inputs on the comments box is welcome.
I have been given this case to solve in an attempts to understand the topic of patient clinical data analysis, to develop my competency in reading and comprehending clinical data including history, clinical finding, investigation.
A 32 year old man had come to the OPD with chief complaints of pedal edema , low urine output and shortness of breath since the past 4 days
The patient used to work as an autodriver and his daily routine consisted of him waking up at 6am and he drove children to school , his average work day ended at 8pm after which he used to have an occational drink with his friends .
7 months ago the patient had headache , dizziness and blurring of vision for which he had gone to a hospital in nalgonda and there he was diagnosed with hypertension and was started on Telma.H and was referred to another hospital where he had gotten a creatinine test done and the level was 8.6 and he was started on Arkamin
he was referred to KIMS for dialysis and had been getting dialysis done since the past 8 months
He developed backpain 4 months ago which was dragging type and was relieved upon rest
History of present illness
pedal edema since one month uptil leg and it subsided on rest
And it now it is till ankle level
There is more marked edema on the right leg compared to left
Decreased urine output since 10 days
And associated with pain when initiating it and passes only 2 to 3 drops
Sob on excertion and subsided on rest
He has cough since 4 days which was non productive
Palpitations are present
he developed backpain 4 months ago which was dragging type and relieved upon rest
on 18th September the patient was referred to the orthopedic department for his backache wherein he was diagnosed with ? at the L4 ,L5 region
no neurological deficits present
History of past illness
a known case of Hypertesion since 1 year
n/k/c/o DM,thyroid,TB
Personal history
occupation : auto driver
diet :mixed
appetite : decreased
bowels : regular
micturition :decreased urine output
no known allergies and no addictions
occasionally consumes 180ml of Alcohol at social gatherings
Family history
his elder brother id a known case of hypertension since 16 years
General Examination
patient was conscious , coherent and coherent and examined in a well lit room
VITALS
pulse rate : 99bpm
respiratory rate : 19/min
BP: 150/80 mmHg
Temperature : Afebrile
GRBS : 127mg%
SpO2: 98% at room temperature
physical examination
Pallor : not present
icterus : not present
cyanosis : not present
clubbing : not present
lymphadenopathy : not present
generalised anasarca is seen
pedal edema : present , pitting type
Systemic examination
CVS
S1 and S2 are heard
no thrills and no murmurs
Respiratory
vesicular breath sounds heard
trachea is in central position
no wheezing
no dyspnoea
on 7th october the patients Oxygen saturation was dropping and reached 40% , so since then the patient has been given humidified oxygen
on 8th october JVP was seen prominently and Rhonchi was heard , the patient was put on nebulization with budecort
Abdomen
obese shaped abdomen
no tenderness
no palpable mass
no hernial orifices
no free fluid
liver and spleen are not palpable
bowel sounds are heard
CNS
Conscious and normal speech
normal gait
crainal nerves are normal
sensory system is normal
motor system is normal
Reflexes
right. left
biceps +2 +2
triceps. +2. +2
supinator +2 +2
knee +2 +2
ankle. +2 +2
INVESTIGATIONS
MRI
Ultrasound report
On 4th September
Ultrasound report
RFT
Complete blood picture
On 5th September
LFT
on 18th sepember
RFT
On 29th September
Complete blood picture
RFT
On 5th October
RFT
Patient images
-generalised edema and pitting edema
Pleural tap (right lung ) was done and fluid aspirated was frothy
on 7th october
raised JVP was seen
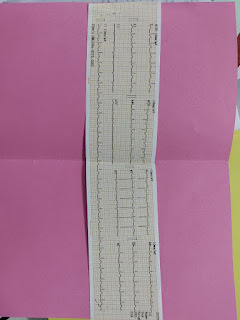
ECG
PROVISIONAL DIAGNOSIS
CKD on MHD secondary to Hypertensive nephropathy
PLAN OF MANAGEMENT:
Renal Transplantion
TREATMENT :
On 5/10/21 :
Fluid restriction <1L/day
Salt restriction <2.4L/day
T.Lasix 40mg PO/BD
T.Nicardia 20mg PO/TID
T.Arkamine 0.1 mg PO/BD
T.Shelcal CT po/od
T.Nodosis 500 mg
T.Met XL 50 mg po/od
INJ erythropoietin 4000 units weekly once
BP monitering
On 6/10/21 :
Fluid restriction <1L/day
Salt restriction <2.4L/day
T.Lasix 40mg PO/BD
T.Nicardia 20mg PO/TID
T.Arkamine 0.1 mg PO/BD
T.Shelcal CT po/od
T.Nodosis 500 mg
T.Met XL 50 mg po/od
INJ erythropoietin 4000 units weekly once
BP monitering
On 7/10/21
Fluid restriction <1L/day
Salt restriction <2.4L/day
T.Lasix 40mg PO/BD
T.Nicardia 20mg PO/TID
T.Arkamine 0.1 mg PO/BD
T.Shelcal CT po/od
T.Nodosis 500 mg
T.Met XL 50 mg po/od
T.Metolazol 5 mg po/ bd
INJ iron sucrose 100 mg iv / bd
INJ erythropoietin 4000 units weekly once
Update on 11th October
Update : 13th October
Patient is getting discharged at 4:00pm
he is advised to come for dialysis on Monday (20th October )
fluid restriction is also advised
14th October
He was admitted again for pain abdomen
A video featuring transpendicular biopsy at L4 level


































Comments
Post a Comment