A 49 year female with HFrEF secondary to? CAD
A 49 year old female came in to casualty with chief complaints of fever since 10 days, cough since 10 days, SOB since 2-3 days, decreased urine output since yesterday.
History of presenting illness:
Patient was apparently asymptomatic 10 days back then she developed
fever which is of incidious in onset, intermittent in nature and is of low grade fever, subsided on taking medication.
cough since 10 days which is associated with sputum and scanty in amount
sob on excertion 5 to 6m months back
Progressed to grade 4 ( at the time of presentation) and worsening.
pedal edema since 5 to 6 months which is associated facial puffiness.
decreased urine output since yesterday night.
H/o covid vaccination 8 days back.
Past history:
k/c/o HTN since 1 year and is on Tab. TELMA-H (40/12.5 MG) - but is Irregular in taking medications.
-? k/c/o kidney disease 5-6 years back but not on any medications.
No history of DM, CAD, asthma, TB, epilepsy.
No h/o similar complaints in the past.
Personal history:
Appetite is normal
Duet is mixed
Sleep is adequate
Bowel and bladder regular
No addictions.
Family history:
No significant family history or allergic history.
General examination:
Patient is c/c/c with moderate built and moderate nourishment.
No pallor, icterus, cyanosis, clubbing, lymphadenopathy, pedal edema.
Vitals:
BP: 179/110 MMHG,
PR: 112,
Temp: 98.6 °F,
RR: 28 CPM,
SPO2: 82%
GRBS: 187 MG%
RS: B/L inspiratory crepts all over lung fields.
CVS: S1 ans S2 heard. No murmurs.
P/A: soft and non-tender.
CNS: No focal deformities.
Investigations:
Hemogram
Hb: 8.2
TLC: 13,300
PCV: 22.2
RBC: 2.95
PLT: 3.41
LFT
TB: 1.13
DB: 0.24
SGOT: 34
SGPT: 27
AP: 327
TP: 5.5
A: 3.5
A/G: 1.85
RFT
UREA: 161
CREAT: 10
NA: 130
K: 4
CL: 90
SEROLOGY : negative.
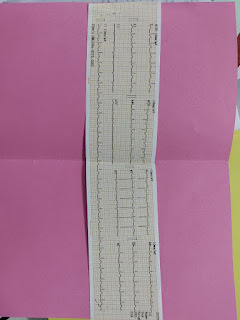
ECG
On 30 September
ULTRA SOUND :
B/L grade 2 RPD.
Left simple renal cyst.
2D-ECHO:
Moderate to severe LV dysfunction ( EF: 35%)
Mixed MR with no MS.
Mixed TR with mild PAH.
Mixed AR with sclerotic AV.
Transient LV dilated.
Diastolic dysfunction.
No PE/LV clot.
RWMA present, Lad akainesia, RCA and LCX hypokainesia.
Provisional diagnosis:
HFrEF secondary to? CAD ( EF - 35%) ( LAD - Akinesia).
-? CKD ( stage 5.)
-? Cardiogenic pulmonary edema.
Treatment:
On 1st October
O2 inhalation @ 6-8 lit min ( if spo2>92%)
Neb & Dubolin and budecort 8th hourly
Inj Lasix 40mg|IV| BD
Inj.PCM 650mg PO sos
Inj. Pan 40mg IV BD
Inj. Zofer 4 mg /IV / sos
Inj cefriaxone 1 g IV BD
T.met- XL 50mg | PO| OD
Tab.Ecosprin~ Av (75/20)mg PO HS
Monitor vitals hourly
GRBS 8th hourly
T. Amlong 20mg PO OD
On 3rd October
Inj hydrocortisone 100mg IV stat
Inj lasix 80mg IV stat
Inj.NTG 2mg IV stat
T.nicardia 20 mg PO stat
Neb. Duolin and budecort stat
Bipap if spo2 not maintaining
Inj neomal 1g IV stat
On 4th October
O2 inhalation (maintain more than 92 percent
Inj.lasix 40mg IV BD
Inj.pan 40 mg IV OD
Inj. Zofer 4mg IV sos
Tab. Pcm 650mg PO sos
Neb duolin and budecort 8th and 12th hr respectively
Monitor vitals hourly
Salt restriction less than 2.4g/day
Water restriction less than 1 lit / day
T. Ecosprin AV (75/20)mg PO
T. Nicardia 20mg po bd
T. Aricamine 0.1mg po tid
She was discharged the following day




Comments
Post a Comment