MEDICINE PRACTICAL EXAMINATION CASE
This is an online e log book to discuss our patient identified health data shared after taking his/her guardian signed informed consent. Here we discuss our individual patient problems through a series of inputs from available global online community of experts with a aim to solve those patients clinical problem with collective current best evidence based inputs.
This blog also reflects my patient centered online learning portfolio and valuable inputs on the comments box is welcome.
I have been given this case to solve in an attempts to understand the topic of patient clinical data analysis, to develop my competency in reading and comprehending clinical data including history, clinical finding, investigation.
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
12 Jan 2022
Rithika.K
MEDICINE CASE DISCUSSION
A 40 year old female came with the complaints of fever since the past 20 days and shortness of breath since the past 3 days along with vomiting for the past 1 day and decreased urine output for the past 1 day.
Patient was a daily wage worker by occupation. She starts her day at 4am and finishes her morning routine by 6am. She consumes alcohol daily, around 750 ml for the last five years which began after her husband passed away.
HISTORY OF PRESENTING ILLNESS:
The patient was apparently asymptomatic 20 days ago, when she had an insidious onset of intermittent fever which was low grade, with an evening rise in temperature. This was associated with chills and rigours, and was relieved on taking medications.
The fever was non relenting, so she was admitted to a local hospital in miryalaguda 3 days back where she was given conservative therapy with antibiotics and analgesics, and then she was referred to our hospital 1 day back.
The patient has been complaining of shortness of breath for the past 20 days. Shortness of breath is present while doing daily activities- Grade 3 (Ex. Washing clothes, cleaning utensils) which gradually progressed to the current state, where the patient has shortness of breath even at rest (Grade 4). This was not associated with orthopnoea, paroxysmal nocturnal dyspnea or pedal edema.
The patient has had two episodes of vomiting which are non projectile, non bilious, non foul smelling and contains undigested food particles.
Patient has had decreased urine output from the past 1 day, associated with burning micturition.
No associated abdominal pain, constipation, diarrhoea, melaena.
She was having hallucinations and self talking behavior and irrelevant talk and is under psychiatric evaluation
PAST HISTORY:
Medical history-
The patient is not a known case of Diabetes Mellitus, tuberculosis, asthma, epilepsy, CAD
She had been diagnosed with hypertension 3 years ago, for which she is not on any medication.
Surgical history-
There is no relevant surgical history for this patient
PERSONAL HISTORY:
Diet- Vegetarian
Appetite- Decreased since the past 20 days
Sleep- Decreased since past 20 days
Bowel and Bladder movements- Urine output decreased for past 1 day, bowel movements are normal
Addictions- Patient consumes alcohol daily for the past five years (750ml per day for the past five years)
She also has a habit of tobacco chewing occasionally for past 2 years.
Her last alcohol intake was 10 days ago
Menstrual history
Age at menarche-12 years
Cycle repeats for every 28 days.
she bleeds for 5 days, uses 5 pads per day, no clots
Family history- not significant
GENERAL EXAMINATION:
The patient was conscious, coherant, and co-operative and well oriented to time, place and person. With prior consent, patient was examined in a well lit room, lying down on the bed. She in thin built and moderately nourished.
Pallor- Present
Icterus- Present
Clubbing- Absent
Cyanosis- Absent
Lymphedenopathy- Absent
Edema- Absent
VITALS-
Temperature- 98.4 F
Pulse rate- 110 bpm
Blood pressure- 110/60 mmHg
Respiratory rate- 36 cpm
Sp02 at room temp- 95%
SYSTEMIC EXAMINATION
Abdominal examination
INSPECTION:
Shape – scaphoid, not distended
Flanks – free
Umbilicus – Central, inverted
Skin- LSCS scar is present, no sinuses, striae are seen
Dilated veins – absent
Movements of the abdominal wall with respiration is present
No visible gastric peristalsis or intestinal peristalsis
PALPATION:
Superficial Palpation
No local rise of temperature or tenderness
Deep Palpation
Liver-
It is palpable in the Right hypochondrium about 5 cms below the Right costal margin in the Mid clavicular line and 2 cms in the midline from the Xiphisternum
which moves with respiration and is firm in consistency with a
Smooth surface and a rounded edge. The upper border of the liver is not palpable.
Spleen-
Spleen is palpable in the Left Hypochondrium, enlarging towards the Right Iliac Fossa
2 cms below the Left Costal Margin in the Mid clavicular line, which moves with respiration and is firm in consistency with a Smooth surface and a rounded edge.
Kidney
It is not palpable
No other Palpable swellings in the abdomen.
PERCUSSION:
Percussion of Liver for Liver Span- The liver span is 16cm from mid clavicular line and 7 cm from sternum dull percussion
Percussion of Spleen- Dull note on percussion
There is no fluid thrill, shifting dullness
AUSCULTATION:
Bowel sounds are heard
RESPIRATORY SYSTEM-
Inspection-
Chest is bilaterally symmetrical
The trachea is positioned centrally
Apical impulse is not appreciated
Chest moves normally with respiration
No dilated veins, scars or sinuses are seen
Palpation-
Trachea is felt in the midline
Chest moves equally on both sides
Apical impulse is felt in the fifth intercostal space
Tactile vocal fremitus- appreciated
Auscultation:
B/l air entry- present
NVBS are heard. No adventitious sounds were heard.
Percussion-
The areas percussed include the supraclavicular, infraclavicular, mammary, axillary, infraaxillary, suprascapular, infrascapular areas.
They are all resonant.
CVS-
Inspection-
The chest wall is bilaterally symmetrical
No dilated veins, scars or sinuses are seen
Apical impulse or pulsations cannot be appreciated
Palpation-
Apical impulse is felt in the fifth intercostal space, 2 cm away from the midclavicular line
No parasternal heave or thrills are felt
Percussion-
Right and left borders of the heart are percussed
Auscultation-
S1 and S2 heard, no added thrills and murmurs are heard
CNS-
HIGHER MENTAL FUNCTIONS:
Patient is Conscious, well oriented to time, place and person.
All cranial nerves - intact
Motor system
Right Left
BULK
Upper limbs N N
Lower limbs N N
TONE
Upper limbs. N N
Lower limbs. N. N
POWER
Upper limbs. 5/5. 5/5
Lower limbs 5/5. 5/5
Superficial reflexes and deep reflexes are present , normal
Gait- Could not elicit, the patient was not able to get off the bed
No involuntary movements
Sensory system - All sensations (pain, touch, temperature, position, vibration sense) are well appreciated.
INVESTIGATIONS
PH- 7.40
PC02- 21.3
P02- 54.7
HC03- 13.0
Serum LDH- 346 IU/L
LFT-
Total bilirubin- 4.7 mg/dl
Direct bilirubin- 2.57 mg/dl
AST- 102
ALT- 35
ALP- 144
Total proteins- 5.6
Albumin- 2.3
A/G- 0.72
RFT-
Urea- 45 mg/dl
Creatinine- 3.2
Uric acid- 8.0
Ca- 10 mg/dl
Na- 136
P- 4.4 mg/dl
K- 4.8 meq/lt
Cl- 90 meq/lt
Coagulation profile-
PT- 20
INR- 2.4
aPtt- 41
Complete urine exam-
Albumin- ++
Sugar, bile salts, bile pigments- normal
Pus cells- 10-12
Epithelial cells- 4-5
RBC- 3-4
Casts- granular casts are present
Complete blood picture-
Reticulocyte count- 0.5%
Hb- 5.7
TLC- 18400
N/L/E/M- 93/4/1/2
PLT- 65000
USG interpretation
Hepatomegaly with mildly altered echo texture
Spenomegaly ( Mild )
Altered echo texture of renal cortex with well maintained cortico- medulary differentiation
2D echo interpretation-
Good left ventricular systolic function
No regional wall motional abnormalities
Right atria mild dilated
Sclerotic atrial valve
Diastolic dysfunction is present
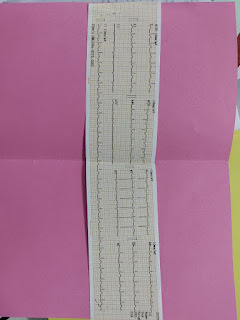
Fever charting
Diagnosis
- fever with hepatosplenomegaly (clinical malaria)
-Severe anemia (hypo proliferation anemia) evaluation
-Prerenal AKI, UTI
-Delirium
12/1/2022
O/E
BP-100/60mg
PR-84/min
CVS-s1 s2 heard
RS- BICAE +
CNS-NFD
P/A-soft
Rx
1)IVF 1-NS(urine output+ 30ml/hr)
-RL
2)INJ PIPTAZ 2.25gm*IV*TID
8am-1pm-8pm
3)INJ FALCIGO 120mg*IV
0-12hrs-24hrs-48hrs
4)INJ PAN 40mg*IV*OD
5)INJ ZOFER 4mg*IV*OD
6)GRBS 6th hrly
8am-2pm-8pm-2am
7)strict I/O charting
8)monitor BP/PR/SPo2 chart 4th hrly
9)temp chart 4th hrly
10)syp.cremaffin plus
11)INJ-vit k 10mg/IV stat
12)INJ THIAMINE 1AMP in 100ml NS
Adv
2d echo
Psychiatry referral
Serum ferritin
24hr urinary protein,creatinine
11/1/2022
O/E
Patient is coherent and cooperative
BP-110/60mmhg
PR-84/min
CVS-s1s2 heard
RS -
CNS-NFD
P/A -soft
Hepatospleenomegaly +
GRBS-86mg/dl
Rx
1)IVF
Urine output +30ml/hr
2)INJ PIPTAZ 4.5 gm*IV*stat
INJ PIPTAZ 2:25gm*IV*TID
3)INJ PAN 40mg*IV*OD
4)INJ ZOFER 4mg *IV*OD
5)GRBS 6th hrly
8am-2pm-8pm-2am
6)strict I/O charting
7)monitor BP/PR/SPo2 monitoring 4th hrly
8)Tab DOXYCYCLINE 100mg*PO*BD
9)INJ FALCFGO 120mg
Adv
Arrange for 1 OPRBC
PSYCHIATRIC REFERRAL (12/01/2022)
Notes include-
Patient has been evaluated and has a provisional diagnosis of fever and hepatosplenomegaly with pre renal AKI and has been referred to psychiatry due to irrelevant talking, hallucinations for the past 2 hours.
History includes that the patient has had a fever for the past 20 days that is not subsiding. Patient consumes around 6 units if alcohol per day for the past five years, after the death of her husband. She experiences sleep disturbances and tremors when she doesn’t consume alcohol. She also has a history of tobacco chewing. Patient has had similar episodes in the past (5 years back) when she was diagnosed with anemia. Self talking stopped 3 days after starting treatment.
History of the episodes-
As per the attending, and doctors present, she suddenly started talking to the walls as if she was talking to a known person standing in front of her.
She says that she can see them and they are talking objectively about her.
Sleep is disturbed but the appetite is normal.
The case notes of the referral are given below,
















Comments
Post a Comment