A 65 year old male with right upper and lower limb weakness
This is an online E-Log book to discuss our patient's de-identified data shared after taking his/her/Guardian's signed informed consent. Here, we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve these patient's clinical problems with collective current best evidence-based inputs. This E-log also reflects my patient-centered online learning portfolio and your valuable inputs in the comment box are welcome.
CASE DISCUSSION:
A 65 years old male came to the OPD with
chief complaints of difficulty in lifting right upper limb and lower limb since 3days.
Deviation of angle of mouth towards right since 3days.
Difficulty in swallowing liquids and solids since 3 days.
History of presenting illness:
Patient was apparently asymptomatic 7 years ago then he had dinner around 8pm and slept, at 2pm he woke up to pass urine then he suddenly fell in the bathroom following which he had right side hemiparesis for which he went to a private hospital and was diagnosed with CVA and HYPERTENSION, given medication and discharged.
The patient took ?medications for 1year and stopped taking them, took physiotherapy for 1 month it took 3months to walk but did not recover completely and since then uses cane to walk.
The patient was started on ANTI HYPERTENSIVES ? which he used for one year.
No slurring of speech during this episode.
No loss of consciousness.
Later he took his medications on and off till 1 year ago since then he completed stopped taking medication.
On 6/02/2022,
Patient went to use washroom around 5am and was not able to get up after passing urine.
Slurring of speech was present,Deviation of angle of mouth towards right,
Dysphagia, right side hemiparesis.
He was taken to a private hospital and was admitted there for three days, took a CT BRAIN impression:
Ill-defined patchy hypodensity in left body of caudate nucleus and left corona radiata - ?subacute to chronic infarct.
Chronic lacunar infarcts in bilateral capusloganglionic regions and bilateral corona radiata.
Diffuse cerebral atrophy.
Chronic small vessel ischemic changes.
Then was referred here for further treatment.
Past history
Not a k/c/o DM, TB, Asthma, Epilepsy.
Personal history of
DAILY ROUTINE before illness:
5am- wakes up and get ready
7am- Tea
10am- breakfast
12pm- goes to work (goatherd)
6pm- come back home and cleans up
8pm- dinner
9pm- sleeps
after illness: patient has the same routine as before, but has difficulty in walking.
Diet- Mixed
Appetite- Normal
Bowel- regular, passed stools 3 days ago ; bladder movements- Regular.
Sleep- Adequate
Addictions- H/o alcohol consumption 90ml/day for 20years 7 years ago ,since then consumes occasionally.
Surgical history- Cataract surgery in both eyes 8 years ago
Family history:
Insignificant
General examination:
The patient was examined in a well-lit room after informed consent was taken.
He is conscious, coherent, cooperative, well oriented to time, place and person. He was well nourished and moderately built.
No Pallor, Icterus, Clubbing, Cyanosis, Koilonychia, Lymphadenopathy, Edema.
Vitals:
PR: 92bpm
RR: 22cpm
BP: 110/90 mmHg
Temperature: 99°F
GRBS: 94mgdL
SpO2: 95% on room air.
Systemic examination:
CNS
HIGHER MENTAL FUNCTIONS:
Oriented to time,place,person
Memory : immediate,recent, remote intact
Speech: slurred
No delusions or hallucinations
CRANIAL NERVES:
1- not tested
2- counting fingers+
3,4,6- No restriction of movement of eye
5-normal( muscles of mastication+sensations of face)
7-deviation of Angle of mouth to right side.
8- Normal hearing
9,10-difficulty in swallowing and slurred speech, gag reflex not tested
11,12- normal.
MOTOR EXAMINATION:
TONE: Increased in right upper and lower limbs and normal in left upper and lower limbs
POWER : Right Left
Upper limb 4/5 4/5
Lower limb 3/5 4/5
Reflexes : Right Left
Biceps: 3+ 2+
Triceps: 3+ 2+
Supinator 3+ 2+
Knee: 2+ 2+
Ankle: - -
Right biceps
SENSORY EXAMINATION:
Pain and touch present
CEREBELLUM EXAMINATION:
Able to do finger nose test.
dysdiadokinesia present
No rebound tenderness
Gait: couldn't walk , CIRCUMDUCTION PATTERN (as patient's attenders described)
AUTONOMIC NERVOUS SYSTEM:
No abnormal sweating
No resting tachycardia
MENINGEAL SIGNS: Absent
CVS: S1 and S2 heard.
RS: BAE+ NVBS+
Per abdomen
Soft, non tender, no distension, umbilicus is central and inverted,no scars, no sinuses.
INVESTIGATIONS:
HEMOGRAM
Hb- 15.4g%
TLC- 8,700 cells/cc
Neutrophils-78
Lymphocytes- 12
Eosinophils-2
Monocytes-8
Basophils-0
PCV-43.7
MCV- 37.8
MCH-30.9
MCHC-35.2
RDW-CV- 13
RDW-SD- 42.5
RBC- 4.98m/cc
Platelets- 2.18lakh
PS- NORMOCYTIC NORMOCHROMIC
LFT
TB- 2.11
DB- 0.94
AST- 41
ALT- 26
ALP- 98
TP- 7.4
ALB- 3.83
A/G- 1.07
RFT
Serum urea- 22
Serum creatinine- 1.1
Na+: 135
K+: 4.1
Cl- 98
SEROLOGY
HIV- NEGATIVE
HBsAg- NEGATIVE
HCV- NEGATIVE
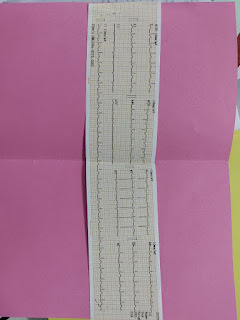
ECG
PROVISIONAL DIAGNOSIS:
Subacute ischemic CVA stroke
TREATMENT:
Tab. CLOPITAB 75mg PO/OD
Tab. ECOSPRIN 75mg PO/OD
Tab. ATORVA 20mg PO/OD
RT feeds 4th hourly 100ml milk and 200ml water
BP/PR/RR/ Temp. Charting 4th hourly
Tab. PAN 40mg PO/OD
Inj. OPTINEURON 1amp in 500ml NS/IV/OD
Right side supinator and brachioradialis
Left kneeRight knee






Comments
Post a Comment