A 78/M WITH ABDOMINAL PAIN AND REDUCED URINE OUTPUT
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.
Chief complaints
Pain abdomen since 2 days
Reduced urine output since 1 day
History of presenting Illness
Patient was apparently asymptomatic 2 days ago then developed pain in right HYPOCHONDRIUM, insidious oncet, gradually progressive not associated with vomitings and not relieved by bending forward position
No history of fever, loose stools, chest pain, palpitations
From 1 day patient is having decreased urine output not associated with burning mituration
Past history
PTCA 10 yrs back
Left-sided hearing loss in 6 years and patient is using hearing aid
Not a known case of diabetes, hypertension, asthma, tuberculosis, epilepsy
Treatment history
Patient is on
1. T. Torsemide 10 mg PO OD
2. T. Isosorbide dinitrite + hydralazine 20/37.5mg PO BD
3. T. Atorvas/clopidogrel 75mg PO HS
VITALS -
TEMPERATURE - 99.1
PULSE RATE - 87 BPM
BLOOD PRESSURE - 130/80 MM OF HG
RESPIRATORY RATE - 30
SPO2 - 97 % AT ROOM AIR
General examination
Patient is conscious coherent cooperative well oriented to time place and person
Pallor +
No Ictrus, cyanosis, clubbing, lymphoadenopathy
SYSTEMIC EXAMINATION -
PER ABDOMEN : DISTENDED, unblicus inverted SOFT, TENDER in Rt iliac fossa, Rt lumbar, rt HYPOCHONDRIUM
CARDIOVASCULAR SYSTEM : S1 AND S2 HEARD , NO MURMURS
RESPIRATORY SYSTEM : BILATERAL AIR ENTRY PRESENT, decreased breath sounds - Rt ISA, IAA, IMA, Fine crepitations Lt ISA, MSA
CENTRAL NERVOUS SYSTEM : NAD
HEMOGRAM
HB 11.9
TC 17,100
PLT 1.88
MCV 86.8
PCV 35.5
MCH 29.5
MCHC 34
SMEAR - NORMOCYTIC NORMOCHROMIC
BGT
A POSITIVE
RFT
Urea 47
Creatinine 2.2
S. Sodium 139
S. Potassium 3.8
S. Chloride 97
Urine chloride 142
Urine sodium 185
Urine potassium 23
Urine protein/creatinine ratio 0.11
S. Amylase 41
S. Lipase 28
CUE
Albumin: trace
Sugar: nil
Pus cells: 2-3
Epithelial cells: 2-3
LFT
TB 1.86
DB 0.94
AST 32
ALT 20
ALP 115
TP 5.7
ALB 3.6
Ultrasound abdomen
Echo of multiple anechoic cyst is noted in both kidneys largest 5.2 X 2.4 cm and the right kidney and 5 X 4.8 CM in the left kidney
Bilateral grade 1 rpd with simple renal cortical cyst
Grade 1 fatty liver
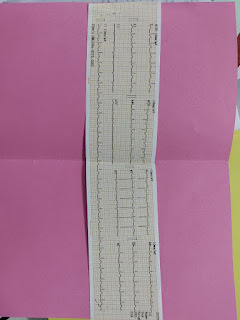
ECG
Chest X-ray
X-ray erect abdomen
ABG
Diagnosis
Acute pancreatitis
with AKI ON CKD
WITH post PTCA (10 yr back)
With Left side hearing loss
Treatment
IVF NS/RL at 50 ml/hr
Inj. Tramadol 1 AMP in 100ml NS IV BD
Inj. Ceftriaxone 1g IV BD
SOAP NOTED DAY 2
ICU bed 2
SOAP NOTES DAY 2
S
C/O abdominal pain decreased
O
VITALS -
Temp - 99.1
PR - 107 BPM
BP - 130/80 MM OF HG
RR - 20
SPO2 - 99% AT ROOM AIR
GE
Patient is conscious coherent cooperative well oriented to time place and person
Pallor +
No Ictrus, cyanosis, clubbing, lymphoadenopathy
SYSTEMIC EXAMINATION -
PA : DISTENDED, unblicus inverted SOFT, TENDER in Rt lumbar, rt HYPOCHONDRIUM
CVS : S1 AND S2 HEARD , NO MURMURS
RS : BILATERAL AIR ENTRY PRESENT, decreased breath sounds - Rt IAA, IMA
CNS : NAD
HEMOGRAM
HB 10.9
TC 6,400
PLT 1.25
MCV 81.6
SMEAR - NORMOCYTIC NORMOCHROMIC, with mild thrombocytopenia
RFT
Urea 78
Creatinine 2.5
2D ECHO
A
HFrEF (EF-34%)
Peripheral vascular disease with cor pulmonale with k/c/o CAD s/p PTCA(10years back) with CKD on conservative management with left sided hearing loss (on hearing aid since 6 years) ?congestive hepatopathy.
P:-
Inj. Lasix 40mg IV SOS if SBP >130MMHG
T. Ecosprin AV 75/10 mg PO HS
T. Met-XL 25 MG PO OD
T. Nodosis 500 mg PO BD
T. Orofer XT PO OD
T. Shelcal 500 mg PO OD
Intermittent CPAP
Inj. Ceftriaxone 1g IV BD (day 3)










Comments
Post a Comment