70yr old male with altered sensorium secondary to ?Meningitis
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 70 Years Old Man Who was a Farmer By Occupation Presented to Casualty With
Altered Sensorium Since 3 Days
Fever Since 20 Days
HOPI :
Patient Was Apparently Asymptomatic Till 2014 ;
2014 - Patient Had Fever Associated with Cough for which he went to Hospital & Was Diagnosed to Have ? Pneumonia with DENOVO DM2 & Was Prescribed with OHAs ( Tab.METFORMIN & Tab.GLIMIPRIDE )
6 Months Back - Patient Had Fever Associated with Cough for Which he Went to Hospital & Said to Have High Sugars along with Lung Infection ; Got Treated & Discharged in a Hemodynamically Stable Manner.Started using insulin for Diabetes Since Then
20 Days Back : Patient Had Fever with Cough ; For Which He went to Hospital & Suspected to Have TB But Reports Turned out to be Negative & Patient Discharged as LAMA & When He Returned Home 3 Days Back He Gradually Developed Altered Sensorium & Couldn't Recognise His Attendants
Past History :
K/C/O DM2 Since 9 Years and on Regular Medications
N/K/C/O HTN ; TB ; EPILEPSY ; ASTHMA
Addictions :
He Started Consumption of Alcohol at the age of 20years & It became a habit to drink 90ml per Day Till 6 Months Back
He Started Smoking Beedis at the age of 20 Years & It Became a Habit to Smoke 20 Beedis Per Day
On Presentation :
BP - 110/80mmHg
PR - 110/min
Temp - 102.5 F
RR - 22/min
Spo2 - 98% @RA
CVS - S1S2 Heard & No Murmurs
RS - BAE + ; NVBS +
P/A - Soft & Non Tender
CNS -
GCS - E2V2M5
RT Pupil - Couldn't be assessed
Lt Pupil - NSRL
Tone - Normal in Both UL & Hypertonia in Both lower limbs
Power - 4/5 In all 4 Limbs
Reflexes - B T S K A - 2+
Plantars - RT - Mute & Left - Flexor
Investigations -
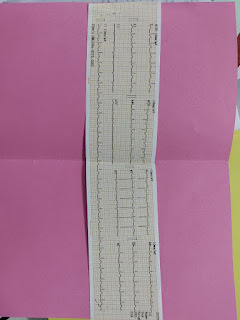
ECG-
S. Urea-24mg/dl
S creatine-0. 8mg/dl
S. Electrolytes -
Na+-132
K+- 3.6
Cl- 98
Ca2+ 1.20
LFT-
Hemogram-
Rbs-157mg/dl
HbA1c-6. 8%
ABG-
CSF analysis-
glucose -42
Protein -60
Cl-121
ADA-131
CSF CELL COUNT
Vol-0. 5 ml
Color- colorless
Appearance- clear
Total count-104 cells
DC-
60% lymphocytes
20% monocytes
20% neutrophils
Others- nil
RBC- nil
Rules tube content
Provisional diagnosis -
?TB meningitis
Treatment -
Ryles tube feeds-200 ml milk every 4 th hourly
100 ml water every hourly
Iv fluids NS @50 ml/hr
Inj. Ceftriaxone 2 GM iv stat
Then inj . Ceftriaxone 1 GM iv bd
Inj Dexa 6 mg iv stat then
Inj. Dexa 6mg iv tid
Monitor vitals 2 nd hourly
Grbs monitoring
Strict input and output charting
Inj. Neomol 1 GM iv /sos ( if temp>101F)
16/02/23
70 year old man c/o fever since 20 days and altered sensorium since 3 days
S-
No fever spikes
Patient obeying to commands
O-
BP - 120/70mmHg
PR - 98/min
Temp - 98F
RR - 22/min
Spo2 - 98% @RA
Grbs-250 mg/dl
CVS - S1S2 Heard & No Murmurs
RS - BAE + ; NVBS +
P/A - Soft & Non Tender
CNS -
GCS - E2V2M5
RT Pupil - Couldn't be assessed
Lt Pupil - NSRL
A-
Altered sensorium under evaluation secondary to? meningitis
?TB meningitis
Investigations -
Hb- 12.0g/dl
TLC- 8700
PLC- 3.02LAKHS
Lymphocytes -32
Pcv-35. 2
S Urea-24mg/dl
S creatine-0. 8mg/dl
S. Electrolytes -
Na+-132
K+- 3.6
Cl- 98
Ca2+ 1.20
LFT-
Total bilirubin-0. 9
ALP-144
Total proteins-6. 2
Albumin-3. 0
Rbs-157mg/dl
HbA1c- 6.8%
P-
Ryles tube feeds-200 ml milk every 4 th hourly
100 ml water every hourly
Iv fluids NS @50 ml/hr
Inj. Ceftriaxone 2 GM iv stat
Then inj . Ceftriaxone 1 GM iv bd
Inj Dexa 6 mg iv stat then
Inj. Dexa 6mg iv tid
Monitor vitals 2 nd hourly
Grbs monitoring
Strict input and output charting
Inj. Neomol 1 GM iv /sos ( if temp>101F)
Inj. HAI S/C according to grbs
17/02/23
70 year old man c/o fever since 20 days and altered sensorium since 3 days
S-
No fever spikes
Patient obeying to commands
Hiccups since yesterday afternoon
O-
BP - 110/70mmHg
PR - 66/min
Temp - 95.5F
RR - 22/min
Spo2 - 98% @RA
Grbs-
15/2/23
8am-250mg/dl
2pm-269mg/dl
4pm-272mg/dl
8pm-278mg/dl
16/2/23
2am - 200 mg/dl
8am - 250mg /dl
2pm 265mg/dl
8pm 140mg/dl
10pm 191 mg/dl
17/2/23
2am 197 mg/dl
8am 175mg/dl
Input-2300ml
Out put-1000ml
CVS - S1S2 Heard & No Murmurs
RS - BAE + ; NVBS +
P/A - Soft & Non Tender
CNS -
GCS - E3V3M5
RT Pupil - Couldn't be assessed
Lt Pupil - NSRL
Tone- normal in all 4 limbs
Power- 4/5 in all 4 limbs
A-
Altered sensorium(resolving) secondary to meningoencephalitis secondary to tuberculosis
K/c/o DM since 9 years
Investigations -
Hb- 11.5g/dl
TLC- 11000
PLC- 3.08LAKHS
Neutrophils -85
Lymphocytes -09
Pcv 34.6
RBC count 3.08
15/2/23
S.Electrolytes -
Na-135
K-4. 3
Cl-102
Ca2+1. 12
P-
Ryles tube feeds-200 ml milk every 4 th hourly
100 ml water every hourly
Iv fluids NS @100 ml/hr
Inj. Dexa 6mg iv tid day 3
Inj human actrapid s/c according to GRBS
Tab. Isoniazid 275 mg (4tabs po/od) morning
Tab. Rifampicin 550 mg (4tabs po/od morning
Tab. Pyrazinamide 1550mg (4tabs po od morning
Tab ethambutol 825 mg po od morning
Grbs 7 th hourly
Inj. neomol 1 g iv sos( if temp >101F)
Strict input output charting
Grbs monitoring
Tab benadone 40mg po/od
Tab baclofen 10mg po/sos
Inj perinorm 10mg iv stat
Inj pan 40mg iv/od














Comments
Post a Comment